Watch Sick – The Battle Against HG here
our story
SICK – THE BATTLE AGAINST HG
Charlotte Howden and Lorne Guy started the Sick film documentary in 2018 after Charlotte decided that she needed to raise awareness of Hyperemesis Gravidarum (HG). HG is a debilitating pregnancy condition that affects 1-2% of pregnant woman, which equates to roughly 3 million women every year.
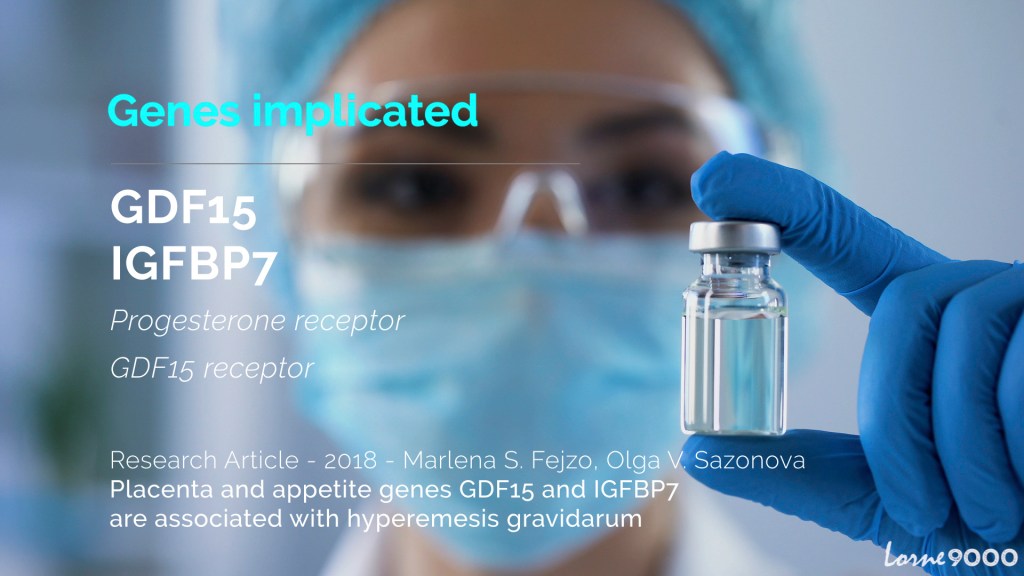
Hyperemesis is simply NOT morning sickness, but a rare most likely genetic condition that causes the sufferer to experience nausea and vomiting on an extreme level – possibly suffering for the whole 9 months of pregnancy. Charlotte herself suffered with HG in 2015 and endured 20 weeks of unnecessary suffering at that hands of this horrific disease but more notably the health care professionals who continued to ignore her.
Without medication or re-hydration in hospital women may suffer life changing consequences from kidney failure, muscle loss and esophageal ruptures to rotting teeth and in some rare cases death.
Charlotte teamed up with Lorne Guy from Good Guys Productions to create a 30 minute short documentary to seek justice and change for the women who are so often passed off as time wasters or dramatic pregnant woman who should be able to handle a little morning sickness. 10% of women with HG terminate their pregnancies….


Sick – The Battle Against HG was released for a 7 day preview on International Hyperemesis Gravidarum Awareness Day in May 2020 to an overwhelming response from sufferers and survivors with over 250,000 views in just 7 days.
Charlotte and Lorne have now made Sick available globally on Prime Video, and Vimeo with more subtitle languages in the works.




Sick is an excellent film resource that will help our members better understand the impact of HG – Gail Johnson, Education Advisor, The Royal College of Midwives
Where can you watch Sick – The Battle Against HG?
To help continue to raise awareness of Sick – The Battle Against HG, Charlotte has launched an HG related podcast series called The Hyperemesis Files podcast. Each week she talks to experts, women and their families who have all suffered with and survived HG. Listen below or direct on Spotify, Google and Apple Podcasts.

CONTACT US
For more information about the film, interview requests or press please contact us via the details below.
Charlotte Howden
e: camberevents@gmail.com
tel: +44 (0)7880 239 565
Lorne Guy
e: lorne@goodguysproductions.co.uk